MRCS Core Knowledge: Compartment Syndrome
28/08/14 07:59 Filed in: MRCS Knowledge
Today’s Wednesday Blog focuses on the commonly tested topic and orthopaedic emergency compartment syndrome.
Background
Compartment syndrome is when intracompartmental pressure exceeds capillary pressure preventing circulation and exchange across vessel walls
If not treated within 4-6hours permanent injury will ensue
Compartment syndrome in diaphyseal tibial fractures is reported to be as high as 45%
Causes:
- Fractures (closed/open)
- Crush Injury
- Tight cast/dressings
- Burns
- Extravasation of IVI
- Bleeding
- Post-ischaemic swelling
Presentation
Pain
- Extreme pain out of proportion to the injury
- Not controlled by opiods
Pain on Passive Stretch (PPS)
- Passive stretch of affected compartment
- Flexor compartment → extension
- Extensor compartment → flexion
Paresthesia
Pulses (LATE SIGN)
- Comparison with non injured
Paralysis (LATE SIGN)
Ulmer et al. showed that:
- Pain, PPS, Parasthesia
- 1 present = 26%
- All 3 = 95%
Pressure Monitoring
Useful in ↓ GCS, polytrauma or to consolidate clinical findings
Normal compartment = 0-10mmHg
A Stryker disposable compartmental pressure probe may be used alternatively an Art. line should be set up, calibrated to the height of the fracture and used. (Describe whichever method is used at your institution).
Under sterile conditions the probe or art line should be inserted into each individual compartment and pressures recorded.
As outlined by McQueen et al a pressure of within 30mmHg of diastolic BP (Δp <30mmHg) or an absolute pressure of > 30 mmHg is indicate of compartment syndrome
Measurements should ideally be within 5cm of the # site
If performed intraoperatively remember that intraoperative diastolic BP is lower than when not anaesthetised
Management
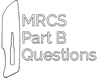
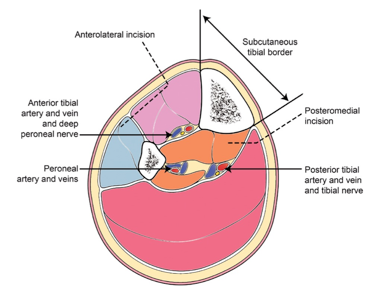
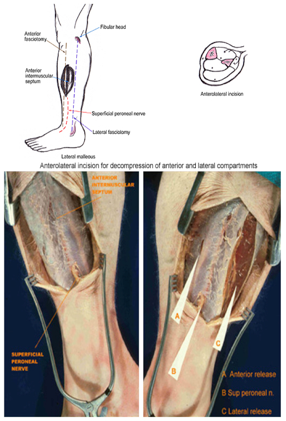
Fasciotomies for lower leg compartment syndrome:
Double incision fasciotomies should be performed to access the anterior and lateral (lateral incision) and deep and superficial (medial incision) compartments. Care should be taken to protect the long saphenous vein (medial) and superficial peroneal nerve (lateral).
Wounds should be left open and dressed with mepatel, gauze and light bandages with patient listed for formal closure in 72hrs.
A detailed guide for incisions can be found in the BAPRAS guidelines on open fractures. Further info on compartment syndrome of other areas can be found in the Question Bank.

References:
McQueen MM, Gaston P, Court-Brown CM. Acute compartment syndrome. Who is at risk? J Bone Joint Surg Br. 2000 Mar;82(2):200-3.
McQueen MM, Court-Brown CM. Compartment monitoring in tibial fractures: the pressure threshold for decompression. J Bone Joint Surg [Br] 1996;78-B
Ulmer T.The clinical diagnosis of compartment syndrome of the lower leg: Are clinical findings predictive of the disorder? Journal of orthopaedic trauma vol.16, no 8, 2002.572-577
Further Info:
For further info and commonly asked questions on compartment syndrome be sure to sign up to the MRCS Part B Questions Bank
blog comments powered by Disqus